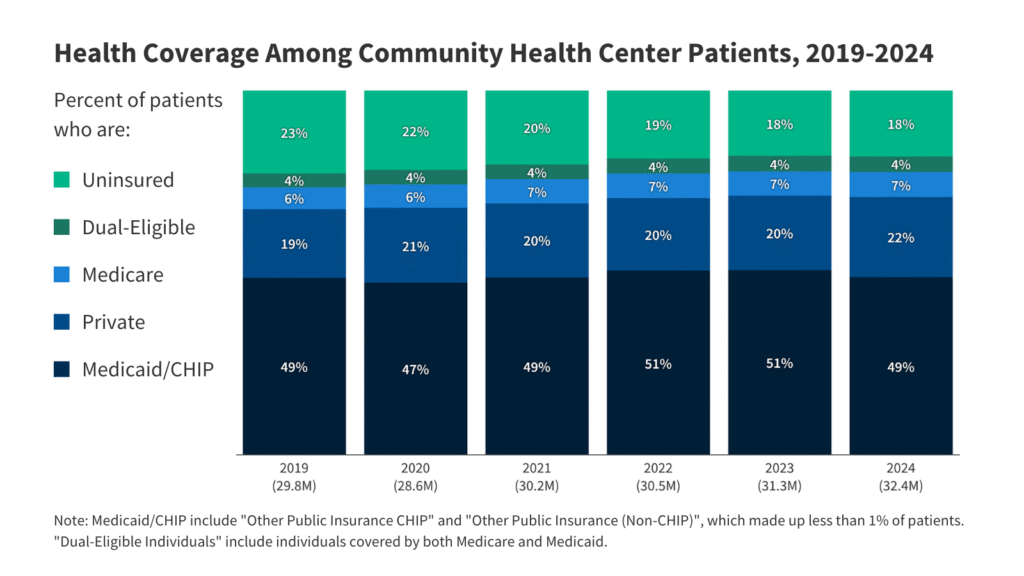
Changes to Medicaid and the ACA Marketplace included in the 2025 reconciliation law are estimated to increase the number of people without health insurance in 2034 by 10 million, which may have an outsized impact on the health center patient population. These coverage losses will be driven primarily by new Medicaid policies like mandatory work requirements for the ACA adult expansion population and the requirement for states to conduct eligibility redeterminations every six months rather than annually, and Marketplace changes, including the elimination of auto renewal and the special enrollment period for people with income less than 150% FPL. These changes are likely to lead to some health center patients losing coverage, even as many health centers provide assistance to patients to help them navigate the new Medicaid and Marketplace rules. Furthermore, changes to Medicaid financing, such as limits on states’ ability to use provider taxes and caps on federal funding for state directed payments to managed care organizations, reduce the federal share of funding, and limit state flexibility in setting provider rates and expanding coverage given ongoing state budget challenges.
Health centers are a primary source of care for immigrant adults, but the 2025 reconciliation law includes eligibility restrictions and make many lawfully present immigrants ineligible for Medicaid and CHIP, ACA Marketplace subsidies, and Medicare. While health centers do not publicly report patient immigration status, data from the 2025 KFF/New York Times Survey of Immigrants show that three in ten (30%) immigrant adults say a health center is their usual source of care, with this share rising to nearly half (45%) of likely undocumented immigrant adults and nearly four in ten (37%) among immigrant adults with limited English proficiency. The law limits eligibility for Medicaid and CHIP, subsidized Marketplace coverage, and Medicare, eliminating coverage for many groups of lawfully present immigrants, including refugees, asylees, and people with Temporary Protected Status, among others. Some states have also reduced or eliminated state-funded coverage designed to fill gaps in federally funded coverage for immigrants due to funding challenges, further reducing coverage options for immigrant health center patients. Reliance on health centers may increase among immigrants who become uninsured as their affordable health care provider options become more limited.
The 2025 reconciliation law also stripped federal Medicaid funding for one year to Planned Parenthood clinics, which may increase demand for family planning services at health centers. This follows actions by the Trump Administration and a Supreme Court ruling that restricted funding to some providers of reproductive and sexual health care services. The share of female Medicaid enrollees who received their last contraceptive visit at a health center across the U.S. was 18% in 2023, with wide variation across states. Health centers may face difficulties in ramping up the availability of family planning services to meet the higher demand if other clinics close.